Executive Summary
Invest for Wellness (i4We), incubated by the Catalyst Group, is a system innovation in primary healthcare, which combines health and wealth interventions, and focuses on wellness for the poor in an affordable, quality assured, and scalable way. The program ensures primary care of members (locally), navigates them through a range of existing secondary and tertiary providers (where required), and uses a blended financing model. The model combines medical, behavioral, and social science with an appropriate mix of technology and health financing. It is currently delivered in four settings: urban, rural, factories, and sex workers’ collectives. i4We has five revenue streams: interest spread on inter-lending among members, sale of health products, fees for citizenry services, sale of insurance, and direct sponsorship of ultra-poor families’ health. These along with a startup grant capital ramp of three to five years enables the program to break even and be self-sufficient.

A daughter waits on her elderly mother, in Bengaluru, India.
Photo Credit: Anup J Kat/Swasti Health Catalyst
Problem
Healthcare does not work for the poor in most parts of Asia, particularly South Asia. The system is unfriendly, or costly, or both. Health is not a priority for the poor, unless it affects their work, and generally only symptomatic relief is sought. This results in repeat episodes of preventable illness and also drug resistance to treatment. The poor lose one to two months of productive time a year due to illness in their family, and nearly 50-60 percent live with some form of undiagnosed illness and die earlier than those economically better off [1]. In India alone, about 50-60 million people in the last decade have been pushed to the brink of poverty because of health-related expenditures [2].
Primary care delivers significant returns and is reasonably simple to implement. However, it has seen few successful models which deliver quality, scale, sustainability, and particularly, address the poorest, with emphasis on prevention and promotion of health. Primary health is not easily monetizable, unlike treatment. Governments generally do a poor job (except in few countries). Many social entrepreneurships have failed in this area, the private sector is uninterested (there is no incentive to prevent), and nonprofit models are often not scalable. Almost none have cracked the balance between prevention and treatment, sustainable funding vs. comprehensive package of services, and community participation vs. payment for services. All of these are key elements for long term success.

An i4We Health Facilitator meets with a member family as part of her routine household visit in Bommanahalli slum in Bengaluru, Karnataka State, India.
Photo Credit: Anup J Kat/Swasti Health Catalyst
Solution
i4We is a self-funded, primary healthcare model, which combines health and wealth interventions, and focuses on wellness for the poor in an affordable, quality assured, and scalable way. The program ensures primary care of members (locally) and navigates them through a range of existing secondary and tertiary providers (where required), and uses a blended financing model, which starts with grant capital and breaks even in five to seven years. It is currently delivered in four different settings: urban, rural, factories, and sex workers’ collectives. The model combines medical, behavioral, and social science with an appropriate mix of technology and health financing. i4We has five revenue streams: interest spread on inter-lending among members, sale of health products, fees for citizenry services, sale of insurance, and direct sponsorship of ultra-poor families’ health. These, along with a start-up grant capital ramp of three to five years, enables the program to break even and be self-sufficient.

An i4We SHG group meeting in Bommanahalli slum in Bengaluru, Karnataka State, India.
Photo Credit: Anup J Kat/Swasti Health Catalyst
How Does It Work?
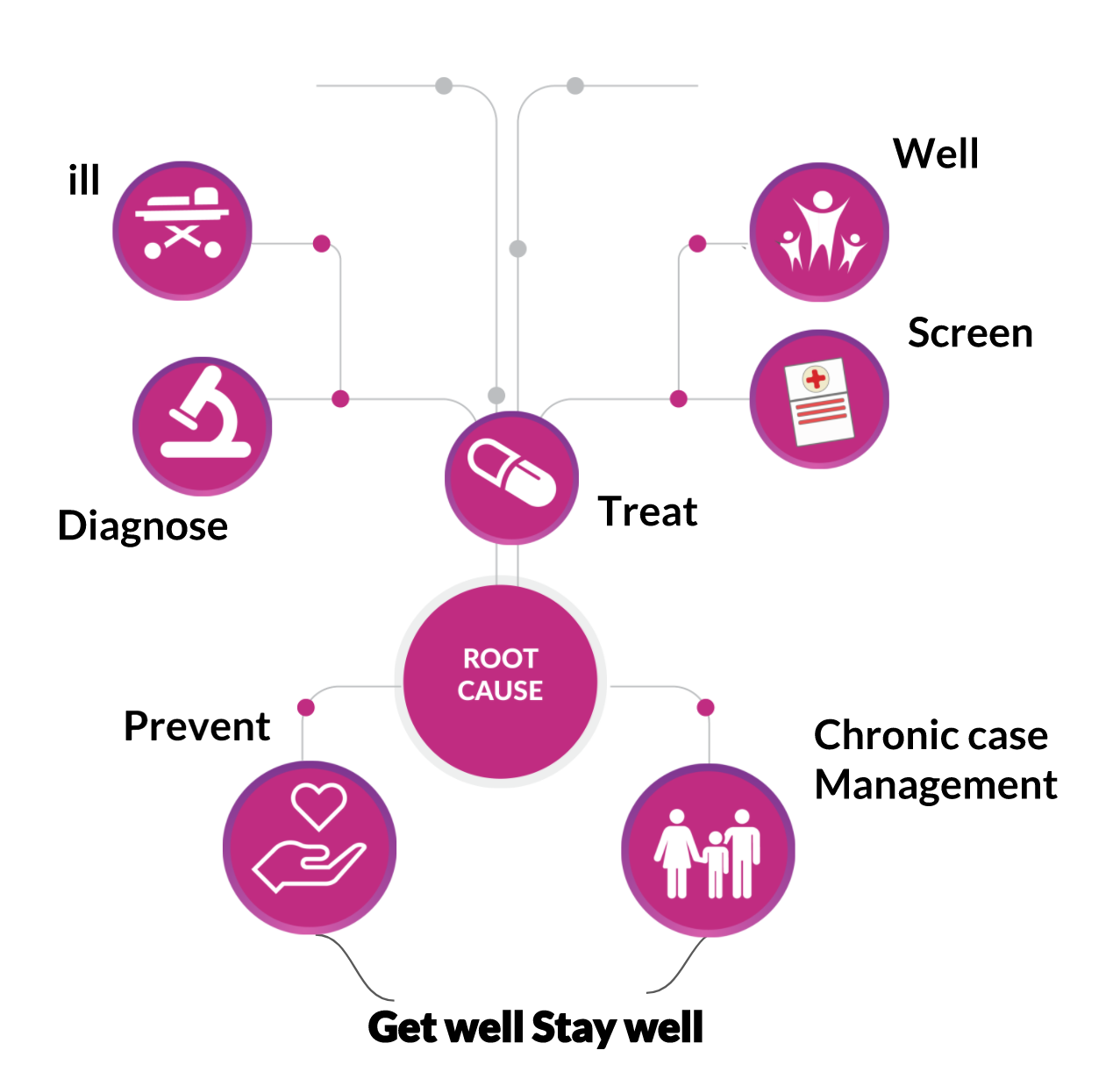
The model works on a membership format. In any setting, a household becomes a member by saving a minimum of ~ 0.8-1 USD per week [3] in a health group (local self-help groups). The diagram below has the ‘Wellness flow.’ When a family member is ill, they get free, prompt, convenient, and empathetic care [4] in the local clinic (by a nurse and dial-in doctor). When they are well, they are screened systematically for 10 high-burden conditions [5]. In both cases, once the treatment is done, the root cause is analyzed and the family is helped with prevention of the next episode. In the case of chronic conditions, continued support to adhere to treatment and other changes are supported.
When the condition is not primary and requires hospitalization or advanced treatment, they are referred to a quality assured network of providers and treatment adherence and completion followed through. The i4We model does not aim to replace any existing health practitioner, instead, it is guided by the philosophy of “work with what works” and complements the existing network of health providers by making them more effective and efficient, with a customer focus.

Women collect potable water from a drinking water plant by Swasti Health Catalyst in Marganakunte village in Chikkaballapura district, rural Karnataka, India.
Photo Credit: Anup J Kat/Swasti Health Catalyst
Members get eight benefits: (a) free treatment in the local i4we Health Center, (b) free insurance for secondary and tertiary care, (c) health mutuals offering reimbursement of out-of-pocket expenses, (d) free screening and treatment for 10 high-burden conditions, (e) access to savings and credit and support groups, (f) free health education and advice (in groups and at home), (g) membership in support groups, and (h) improvement in community situation on Sanitation, Air, Water, and Food (SAWF), key health determinants, through community action.
Uniquely, the program seeks to prevent illnesses and its effects through: (a) Continuously building women SHG (family) members as first responders; (b) Analyzing root cause (when illness is treated successfully) and helping families make changes; (c) Promoting systematic immunization; (d) Screening and treatment for high burden conditions; (e) Promoting health products (like sanitary napkins); (f) Support groups to deal with chronic illnesses, violence, and addictions; and (g) Improving key determinants of health at the community level. The program removes every excuse and impediment for not improving wellness -- systematically, and in a customer-focused way.
i4We uses a strong technology strategy which includes an app for the health facilitator, nurse, and the healthcare provider network, AI enables real time analysis and dashboards for action, point of care diagnostics, and a range of innovative health products. It also uses the latest behavioral science theory and practices including survival analysis, nudge, and other tools.

An i4We Nurse attends to a young boy at the i4We Clinic in Bommanahalli slum, Bengaluru, Karnataka State, India.
Photo Credit: Anup J Kat/Swasti Health Catalyst
For every 5,000 families, a team of 20 Health Facilitators, one nurse, one program manager, and a dial-in doctor, deliver preventive, promotive, and curative aspects of primary healthcare. Every cluster of 5,000, has about 500-600 SHGs and one Health Trust, where SHG leaders and local community leaders govern the program.
The program is designed and implemented with a clear customer (member) focus with every service and product carefully crafted and continuously adapted to local realities. Members can at any time stop being members, which is in itself a feedback on services. By depositing 0.8-1 USD, the members are not paying a user fee -- rather they are saving for themselves, as this capital is returnable on demand at any time. Interest spread on inter-lending (along with other revenue streams) is used for the program costs, which are also governed by the SHG leaders.
Scaling and Impact
i4We is modularized (through technology tools and strong documentation) with inbuilt processes, tools, and methods that are led by a framework, with teams having flexibility in the approach but accountability for results. Agile implementation at scale is enabled with a “plug-in” and work flow approach for each component. A “primary healthcare landscape” exercise that Swasti ran for 10 years (and continuing) provides an arsenal of tools, which have proven to work in many contexts, and enables us to build on what works. The program which began in urban settings is already being adapted by our partners into other settings, rural, factory, sex workers’ collectives, schools, etc., due to its ability to be an easy add-on to existing program and community aggregations/outreach. The program is already expanding from India to Sri Lanka, Lesotho, and potentially Botswana.

An i4We member family from Bommanahalli slum in Bengaluru, Karnataka State, India.
Photo Credit: Anup J Kat/Swasti Health Catalyst
We aim to scale the model to 100 intervention sites reaching 2.5 million people by 2020. This will mean that more than 1.25 million conditions, including anaemia, diabetes, hypertension, and thyroid among others, will be either prevented and/or treated. i4We aims to increase healthy days (by reducing unhealthy days by 30 percent), reduce undiagnosed conditions (by 30 percent), and deliver an independently certified Social Return on Investment (SROI) of 300 percent for its investors.
Started in 2017, the model is operational in five locations in India, covering 36,000 people and growing rapidly. We seek to impact 100 million households and help ensure special communities to “Get Well, Stay Well.” The program was co-created with a range of partners including Vrutti (a livelihood resource center), Catalyst Management Services, Marks & Spencer, Levi Strauss & Co., Social Venture Partners, and World Health Partners among others.

A mother and child from an i4We member family in Bengaluru slum, Karnataka State, India.
Photo Credit: Anup J Kat/Swasti Health Catalyst
In the longer run, the program has the potential to (a) achieve a significant reduction in the mortality and morbidity, (b) empower communities to take charge of, and realize, their health rights, (c) address the needs of the poor and marginalized populations, (d) create a pathway for entrepreneurs and product solutions to reach markets, (e) serve as a model for a comprehensive, integrated, healthy health system that address social determinants of health, (f) set standards in primary healthcare technology solutions, and (g) create a market for prevention with outcomes that the government and donors are willing to buy. Most importantly, our goal is a self-propelled, viable primary healthcare model that can effectively break the cycle of ill-health and the poverty.
Risks
The program needs a time period of three to five years to demonstrate value, it will require donors to be progressive, and true patient capital to be deployed with largely SROI interest. For instance, if scale is measured in terms of the number of people reached instead of the depth of the intervention and outcomes, it can lead to a dilution of the program purpose. Government interference due to a lack of understanding of the model delivery mechanisms, such as on providing treatment without a doctor, can be a risk. Informal providers can feel threatened due to loss of business as i4We Clinic gains membership and value in the community. Another challenge could also be incentivizing continued participation in the program since as people get healthier, they may see a decreased value with reduced number of health incidents. All of these risks are continuously measured and mitigated.
Endnotes
- Gabert et al. Identifying gaps in the continuum of care for hypertension and diabetes in two Indian communities, BMC Health Services Research (2017), 17:846 DOI 10.1186/s12913-017-2796-9
- Tracking universal health coverage: 2017 global monitoring report. World Health Organization and International Bank for Reconstruction and Development / The World Bank; 2017. License: CC BY-NC-SA 3.0 IGO.
- For the ultra-poor, defined in local terms, usually 10% of any local populace, we have a sponsorship model
- The conditions treated include Fever, Cold, Aches/pains, Diarrhoea, Rash, Cough, Dizziness, Fatigue, Discharge, and Wounds.
- The ten high burden conditions that are screened and treated include Anaemia, Vision, Diarrhoea, Blood sugar, Lung diseases, Gender Based Violence, Breast cancer, Oral diseases, Thyroid, Vector borne diseases, and Sexually Transmitted Infections.
Author Bios

Shiv Kumar is the founder and Chief Mentor of Swasti Health Catalyst. He has more than 26 years of experience in more than 30 countries globally, as a founder of several organizations. He has delivered results in the development of programs, and contributes to shaping policies to improve the quality of life for the poor and marginalized. He leads the i4we system innovation effort in primary healthcare.

Priya Pillai is a specialist in gender and public health with a decade of experience in working with communities of women, adolescent girls, and sexual minorities to deliver social impact. She is a creative storyteller who thrives and is excited by the intersection of ideas and actions.


