Introduction
POPULATION HEALTH recognizes the challenges of incorporating social and environmental factors into health services. The current and increasing health care workforce gap and population inequities serve as multiple barriers to Universal Access and Equitable Health Care. The urgency to resolve population health issues is not new. However, in recent years there is an increasing awareness that the main stakeholders in the health sector, along with the community, should improve their contributions for greater quality, equity, relevance, and efficiency in health care delivery. To this end, a unity of purpose must link key health actors. To meaningfully mobilize talents and resources, a clear understanding and recognition of the role of all members of the health team and community, along with culturally sound best practices must be established.
COMMUNITY HEALTH, prioritized by The Network: Towards Unity for Health (TUFH), focuses on effective approaches to serve and engage remote and rural, indigenous, migrants and refugees, women, and elderly populations.
Remote and Rural Health experts consider that remote populations are smaller, more isolated, and more highly dispersed. Central political power is weaker in remote areas; the nature of economic activity varies between rural and remote areas; and socioeconomic disadvantage is higher. As a result, morbidity and mortality are generally worse in remote areas. There are also workforce supply problems and decreased access to health services in remote areas. Different models of service delivery have developed in response to these conditions. Remote areas rely more heavily on visiting services, with differences in the relative roles of health professionals. In remote areas there is a stronger emphasis on public health approaches.
Indigenous populations, according to WHO, are communities that live within, or are attached to, geographically distinct traditional habitats or ancestral territories, and who identify themselves as being part of a distinct cultural group, descended from groups present in the area before modern states were created and current borders defined. They generally maintain cultural and social identities, and social, economic, cultural, and political institutions, separate from the mainstream or dominant society or culture.
Migrant and Refugee Health experts (WHO) indicate that more people are on the move now than ever before. There are an estimated one billion migrants in the world today of whom 258 million are international migrants and 763 million internal migrants -- one in seven of the world’s population. This rapid increase of population movement has important public health implications, and therefore requires an adequate response from the health sector. Ratified international human rights standards and conventions exist to protect the rights of migrants and refugees, including their right to health. Nevertheless, many refugees and migrants often lack access to health services and financial protection for health. The WHO Promoting the Health of Refugees and Migrants Draft Global Action Plan, 2019–20231 identifies six priorities:
- Priority 1. Promote the health of refugees and migrants through a mix of short-term and long-term public health interventions;
- Priority 2. Promote continuity and quality of essential health care, while developing, reinforcing, and implementing occupational health and safety measures;
- Priority 3. Advocate the mainstreaming of refugee and migrant health into global, regional, and country agendas and the promotion of: refugee-sensitive and migrant-sensitive health policies and legal and social protection; the health and well-being of refugee and migrant women, children and adolescents; gender equality and empowerment of refugee and migrant women and girls; and partnerships and inter-sectoral, inter-country and interagency coordination and collaboration mechanisms;
- Priority 4. Enhance capacity to tackle the social determinants of health and to accelerate progress towards achieving the Sustainable Development Goals, including Universal Health Coverage;
- Priority 5. Strengthen health monitoring and health information systems; and
- Priority 6. Support measures to improve evidence-based health communication and to counter misperceptions about migrant and refugee health.
Women Health experts (WHO) indicates that being a man or a woman has a significant impact on health, as a result of both biological and gender-related differences. The health of women and girls is of particular concern because, in many societies, they are disadvantaged by discrimination rooted in sociocultural factors. Some of the sociocultural factors that prevent women and girls from benefitting from quality health services and attaining the best possible level of health include:
- unequal power relationships between men and women;
- social norms that decrease education and paid employment opportunities;
- an exclusive focus on women’s reproductive roles; and
- potential or actual experience of physical, sexual and emotional violence.
While poverty is an important barrier to positive health outcomes for both men and women, poverty tends to yield a higher burden on women and girls’ health due to, for example, feeding practices (malnutrition) and the use of unsafe cooking fuels (COPD).
Elderly Experts Health experts (WHO) indicate that populations around the world are rapidly aging. Aging presents both challenges and opportunities. It will increase demand for primary health care and long-term care, require a larger and better-trained workforce, and intensify the need for environments to be made more age-friendly. Yet, these investments can enable the many contributions of older people -- whether it be within their family, to their local community (e.g. as volunteers or within the formal or informal workforce), or to society more broadly. Societies that adapt to this changing demographic and invest in Healthy Aging can enable individuals to live both longer and healthier lives and for societies to reap the dividends.
To ensure adults live not only longer but healthier lives, a Global Strategy and Action Plan2 on Aging and Health was adopted in May 2016 by the World Health Assembly. This Strategy focuses on five strategic objectives and is a significant step forward in establishing a framework to achieve Healthy Aging for all. It includes a call for countries to commit to action, and develop age-friendly environments. It also outlines the need to align health systems to the needs of older people, and the development of sustainable and equitable systems of long-term care. It emphasizes the importance of improved data, measurement, and research, and involving older people in all decisions that concern them.
Problem
POPULATION HEALTH: The UN High-Level Meeting (UN HLM) on Universal Health Coverage : “Universal Health Coverage: Moving Together to Build a Healthier World” seeks to integrate the “the entire health agenda under the umbrella of Universal Health Coverage (UHC) and sustain health investments in a harmonized manner.” The objective is to raise awareness of the importance of investing in health workforce education that is oriented towards meeting the needs, as well as in tracking and assessing, the impact of education to ensure policies, strategies, and approaches are aligned and optimized to improving quality, relevance, equity, and cost effectiveness of health service delivery. Addressing the health workforce shortage, maldistribution, and performance challenges is essential for progress towards all health-related goals, including Universal Health Coverage. Furthermore, the health sector has the potential to be a driver of economic growth through the creation of qualified employment opportunities, in particular for women. There is growing recognition that CHWs and other types of community-based health workers are effective in the delivery of a range of preventive, promotive, and curative health services, and that they can contribute to reducing inequities in access to care.
COMMUNITY HEALTH recognizes that effective approaches to serve and engage remote and rural, indigenous, migrants and refugees, women, and elderly populations, are often contrary to mainstream health policy, are often ignored, and not included, or recognized in global, national, regional policies and practices that inform mainstream practices.
Solution
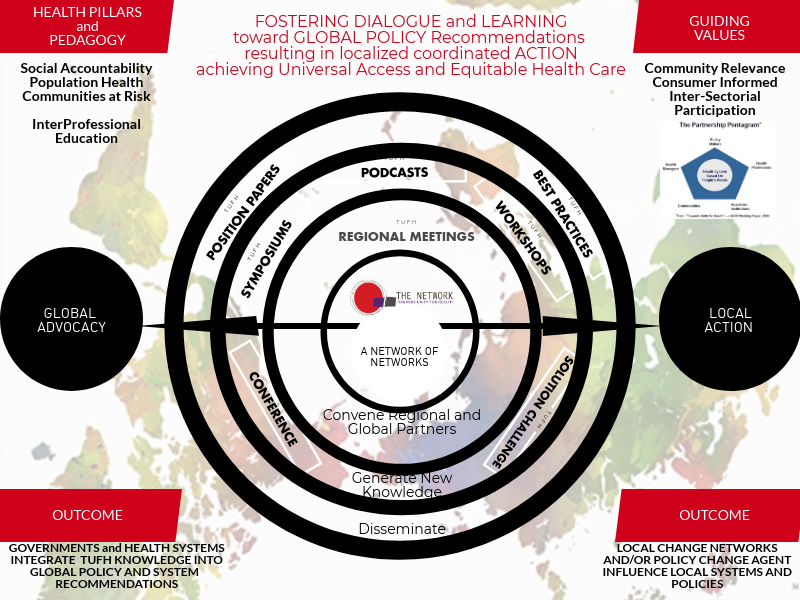
The beginning of moving global systems and policy change to local action starts with inspiring individuals and/or institutions through the sharing of ideas and success of others. Below outlines a three-step model, using network relationships as a strategy, to move global systems and policy recommendations toward local action.
Step 1: Knowledge Sharing
The Network: Towards Unity for Health (TUFH) is serving as a platform to share and distribute best practices and success from countries around the world that have made progress in tackling and implementing ideas regarding Social Accountability and Population Health. The Network: Towards Unity for Health (TUFH), a non-state actor in official relations with WHO believes that relationships are not only between organizations, but between people based around common interests. These relationships are not static, but rather grow and develop from new members and future generations. A key element of The Network: TUFH is that it is not an insular organization. It is an ever evolving and inclusive network that embraces other organizations that are striving to create educational best practices, share community health approaches, and partner on research to develop the evidence for what works.
The articles on Population and Community Health contained in this edition represent case studies and success stories. Through the sharing of ideas and stories we inspire others to consider adoption and adaptation of the ideas and model for local change.
Step 2: Building Local Capacity
The road to global adoption and implementation is long and arduous. TUFH believes that the sharing of knowledge in the form of research and implementation best practices leads to inspiring local change agents to take action. Once inspired, local change agents can be supported by international and peer-to-peer policy and system change leaders and institutions whose primary role is to build their capacity and provide continual support and adaptation.
Building the capacity of local change agents takes the form of introducing a systems and policy change framework, providing formal opportunities to adapt the framework for a local context strategy, and providing continual support and adaption by and with other change agents across the globe. Networks, such as TUFH, being independent of local actors serve in the capacity of a convener and filling any knowledge gaps that might exist to create a culture that is supportive and learning based.
Step 3: Replication
The third step of moving global systems and policy change toward Universal Health and Equitable Health Care is to ensure there are community-to-community sharing platforms. As one community innovates and/or experiences success, networks such as TUFH, must ensure this knowledge is communicated and shared to other communities who have similar goals. Related to Population and Community Health, below outlines two examples for local replication via model adoption. S i
- Local actors adopt, adapt, and implement the successful integration of Community Health Workers into the Health Care Team.
- Local actors inspired by successes in serving and engaging remote and rural, indigenous, migrants and refugees, women, and elderly populations in other countries adopt, adapt, and integrated them into their own systems.
Conclusion
To bridge the gap between good intentions and government or institutional transformations, organizations such as TUFH must continue to serve as the link and connector between global policy organizations and local change agents such as policymakers, institutions, and associations who are doing the work on the ground. The work of TUFH and similar organizations continues to foster dialogue, build global consensus, grow the capacity of local change agents, and create platforms for knowledge to be shared and distributed. Collectively, we can change healthcare, but we first have to change the conversation.
Footnotes
1 https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_25-en.pdf?ua=1
2 https://www.who.int/ageing/en/
Endnotes
i apps.who.int/iris/bitstream/handle/


