Summary
The scope and aim of this study are to review our experience in maternal mortality reduction in Gezira State, Sudan. The major health project was initiated by the University of Gezira, Sudan in 2005, as a low resource setting in Africa. The evidence was related to village midwives, rural hospitals, causes of maternal mortality, available obstetrics resources, equipment, manpower, and training in all hospitals in the region. Interventions led to remarkable reductions in the maternal mortality ratio. The Safe Motherhood initiative is an ideal program of social accountability for a medical school to support their community’s needs in scientific way.
Introduction
Maternal mortality resulted as a consequence of complications related to pregnancy and birth. Many complications exist before pregnancy and become worsened during pregnancy. About more than 80% of maternal mortalities are due to obstetrics hemorrhaging, infection, hypertension, and unsafe abortion (1). Maternal death is defined as "the death of a woman while pregnant or within 42 days of temination of pregnanc y, irrespective of the duration or location of pregnancy, from any cause related to or aggravated by pregnancy or pregnancy, but not from accidental causes" (2).
The high maternal mortality (MMR) rates in some areas consistently reflects the imbalance in health services and the gap between the nations based on the poor and rich divide. More than 90% of the maternal mortalities (MM) take place in low- or middle-income countries, with the majority occurring in the World Health Organization (WHO)-African Region (3). Of these, the majority were due to direct obstetrics causes related to pregnancy, delivery, or postpartum complications (4).
This study reviews our experience in maternal mortality reduction in Gezira State, Sudan, in the major health project initiated by the University of Gezira, Sudan in 2005. Also, to provide recommendations from this experience for other areas with low-income countries.
Case study and successful story: The University of Gezira Initiative for safe motherhood and childhood
(UGISMC)
The initiative was released by the vice chancellor of the University of Gezira in Feb 2004. Its main objective was to reduce the maternal mortality rate (MMR) and the newborn mortality rate (NMR) in the Gezira state by at least 50%
within five years. The justifications, specific objectives, process of project design, strategies, implementation, and methods of evaluation were described by experts in the field (5).
The main objectives were upgrading of ante-natal care, intrapartum care, puerperal care, and care of the newborn; with emphasis on the intrapartum care (6).
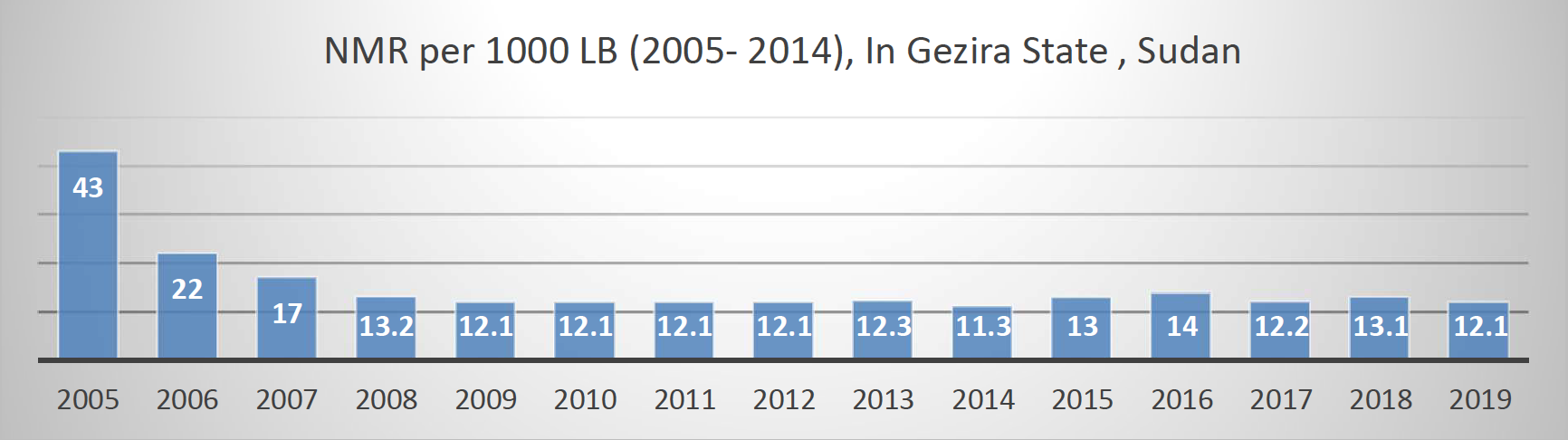
The main strategies were strong political commitment and full partnership with the ministry of health (MOH) at all stages. By the end of 2011 and despite considerable challenges, objectives have been exceeded; the MMR dropped from 469 to 151/100,000 live births and the NMR dropped from 43 to 12/1000 live births Although the reduction in mortality was mainly due to the combined efforts of the initiative and the MOH, other effective factors-namely the overall socioeconomic development in the state must have contributed to that reduction (6).
Settings
The UGISMC was conducted in Sudan. Sudan is a country in the Nile valley of north Africa. It is the third largest country in Africa. Sudan suffers from several challenges including internal conflicts and two civil wars. The population was recorded to be nearly more than 30 million. Gezira, where UGISMC conducted, is a state in Central Sudan. Gezira, and is one of the 18 states of the Sudan. It has an area of 27,549 km2 and is a well populated area, with an estimate population of three million.
Evidenced-based Interventions
This particular project, among other things, initiated the training of village midwives and facilitated their absorption into the government-funded health system, upgrade of the rural hospital, offering of emergency obstetrics services, training on delivery care, and neonatal care in rural hospitals, and manuals and protocols for management of obstetrical & neonatal emergencies and evaluation. All maternal deaths were reviewed retrospectively since the initiative produced.
The first evidenced obtained from the assessment of obstetric resources in all rural hospital (40 hospitals) (7). The comprehensive field survey was conducted and the assessment was made by direct observation in the presence of the hospital director including theaters (major and minor), labor room, human resources assessed, and evaluations. The assessment results of the main five specialized hospitals indicated that all the hospitals can performed the emergency obstetrics care services safely. However, only 33% of the rural hospitals can perform the obstetrics emergencies safely (cesarean section) (7). The results and evidences obtained from this study used to prepare the major project (UGISMC) aim of reducing the maternal mortality in the region by 50% in five years.
Evidence regarding the village midwife (VMW) in Gezira State indicated that about more than 80% of deliveries take place in the home by VMW (8). Hence the concentration on the upgrade the midwifery training and to direct the efforts towards VMW. According to the reports of the state ministry of health, unfortunately 43% of all villages in the Gezira
state lack VMWs (total number of villages=2787; total number of VMW =1583, coverage=75%) and the basic training has been stumbling for the last few years. In 2011 the MOH founded three midwifery schools to rectify the shortage. The initiative had a significant contribution in upgrading the VMWs through support, supervision, and training. The issue of the appalling economic status of the VMW has been addressed several times during the annual meetings of the initiative calling the policy makers attention to it. The initiative struggled at all levels to post VMWs in permanent paid governmental jobs and eventually succeeded. The Gezira State posted 1,000 VMWs and promised to post the rest. That was a major and historical support to VMWs initiated by the initiative and there is evidence that other states are following. The initiative established the in-service training course for the VMWs, which is considered the most effective intervention for improving midwifery services.
Significant evidence obtained from review of maternal mortality in Gezira State in 2016 showed that out of 489 cases of maternal mortality, 113 (23.1 %) were due to postpartum hemorrhage (PPH) as the causative factor. Uterine atony was found to be the main cause leading to 91/113 cases (80.5%) of PPH (9). This important data is consistant with the previous findings of the scientific reports from the ministry of health, professional societies, and UGISMC. However, it’s a preventive cause of MM (PPH) and is an important obstetrical emergency that occurred after birth and represented one of the leading causes of maternal mortality worldwide, including low-income and high-income countries, as well as leading the cause of intensive care unit (ICU) admission (10).
The highest rate was reported in Africa (27.5%) and the lowest rate reported in Oceania (7.2%), the worldwide rate was 10.8% (21) and, in developed countries it is around 13% (20). Risk factors associated with PPH are multiple pregnancies, primigravida, grand-multiparity, and all conditions associated with an over extended uterus (11).
The PPH Project identified the following strategies to decrease maternal death due to hemorrhage: improving maternal health care services, promoting medical and midwifery education and training, aggressive practice of PPH guidelines, early pharmacological intervention, and uterotonic agent’s administration following baby’s delivery. With this background, the PPH Project requested technical assistance from Jhpiego-an international, nonprofit health organization affiliated to with Johns Hopkins University USA. In coordination with the Sudanese American Medical Association, Jhpiego conducted the first HMS –BAB training for Gezira State from February 25 to March 5, 2016. The Master Trainer Course was held at the UofG followed by Champion courses and Clinical Mentor orientation sessions in five hospitals (four rural and one urban). There are an additional five hospitals in Gezira State where providers have yet to receive the Champions course (12). The PPH project should facilitate adherence to HMS training standards including trainer-to-participant ratio, use of effective facilitation and co-facilitation skills in both classroom and in clinical settings, where flexibility and innovations are required, and plan accordingly.
The Rural Hospitals
It is obvious that the whole system of effective maternity care capable of reducing maternal mortality and newborn mortality has to be built around ante-natal care (ANC) and the first referral level of care-is the forty rural hospitals. The upgrading of the rural hospital to one with optimum standards which permits the provision of safe management of obstetric emergencies is a fundamental strategy of the initiative. The upgrading includes rehabilitation of the premises, provision of essential equipment and instruments, posting of adequate numbers of health professionals -- especially consultants, and improving the hospital management. The initiative adopted a clear process to attain those objectives. Early in the project the resources and manpower situation in all of the hospitals were assessed by direct observational visits and the deficiencies were identified by baseline data (7). Approximately 57.6% of the objectives were achieved. The number of hospitals in which a caesarean section could be performed safely increased by 75%, from 16 hospitals in 2004 to 28 hospital in 2011 (65% of the hospitals can perform caesarean section safely) (7). The number of hospitals and
their geographical distribution is adequate, however 31 hospitals need rehabilitation and 12 need rebuilding. Remarkable improvements in the operating theaters; 20 new theaters were built, and the condition of 70%
(30/43) of all theaters is satisfactory. The situation of all health professionals is excellent, 16 obstetricians and 11 pediatricians were posted. Unfortunately, the anesthetic services are still below the optimum standard. The labor rooms are deficient in equipment and instruments; most of them could be easily provided by the hospital itself. In addition, 17 hospitals lack ambulances (40.7%) and the standard of the doctors' houses is poor. The management of all hospitals needs to be strengthened.
Implementation Process
The initiative has been fully committed to its approval process of the implementations. Relationships with the Gezira State governor and government, MOH, professional societies, organizations, and the community at large continue to be reinforced. The committee of the initiative held regular meetings twice per year-- a total of 28 meetings. Each year a detailed plan of action was set and the achievements of that plan and the constraints which it faced were discussed with transparency in the annual meetings which were attended by most stakeholders. A core committee of 10 members was responsible of the follow-up of the plan of action. The evaluation system introduced by the initiative is functioning and nearly all deaths have been reported and audited. The initiative is now fully established in an equipped office in the Faculty of Medicine University of Gezira, Wad Medani.
The Main Strategies in Reducing MMR and NMR
Based on the information obtained from the MOH records, the results of scientific studies, the community surveys, and the opinions of experts, the project committee identified the intra-partum care as the most effective strategy in reducing MMR and NMR and hence the design of the project was tailored towards the upgrading and strengthening of the rural hospital and the VMW.
The majority of obstetric complications are difficult to prevent; placenta previa, pre-eclampsia, malpresentations, and malposition, etc. However, the mortality and morbidity from those obstetrics problems could be reduced by early diagnosis during the ante-partum period and provision of appropriate and skillful intra-partum management.
Almost all of the obstetric complications require hospital treatment. NAC remains one of the essential interventions in reducing MMR and NMR, only if it is supported by well-equipped and efficient system of intra- partum care. The Gezira state reports showed that the coverage and quality of ANC services in State are quite satisfactory.
Village Midwife responsible for the home deliveries in more than 80%. Refer all complicated cases to the first referral level. The rural Hospital-provides emergency management for obstetric complications. One out of every 10 pregnancies require operative delivery and emergency management. Without the first referral level reduction in MMR and NMR can never be achieved.
The ability of intra- partum care to support ANC and reduce MMR and NMR heavily depends on two components are trained personnel (midwives and doctors) and equipped facility (rural hospital). The current situation of the VMWs and the rural hospitals is far below the optimum standards and hence the Safe Motherhood Project emphasizes the upgrading of the intra-partum care as the most effective strategy in reducing MMR and NMR.
Based on the information obtained from the MOH records, the results of scientific studies, the community surveys, and the opinions of experts, the project committee identified the intra-partum care as the most effective strategy in
reducing MMR and NMR and hence the design of the project was tailored towards the upgrading and strengthening of the rural hospital and the VMW through: (i) Rehabilitation of rural hospitals, (ii) Appropriate training, (iii) Supervision, (iv) Continuous monitoring and (v) Periodic evaluation.
Maternal and Neonatal Mortality Reduction
The Gezira initiative has led to a remarkable reduction in the maternal mortality ratio (MMR) and in the neonatal mortality ratio (NMR) in Gezira State. The effort has recorded great achievements in Gezira, lowering the MMR from 469 per 100,000 live births in 2005 to 139 in 2019 (figure 1), and the NMR from 43 per 1,000 live births in 2005 to 12.1 per 1,000 in 2019 (Figure 2). The top six causes of maternal mortality were obstetric hemorrhage (23.3 %), viral hepatitis (19.2 %), pulmonary embolism (15.1 %), eclampsia (13.7 %), sepsis (12.3 %), and malaria (5.5 %).
Figure 1: MMR per 100,000 LB (2005- 2019), In Gezira State, Sudan
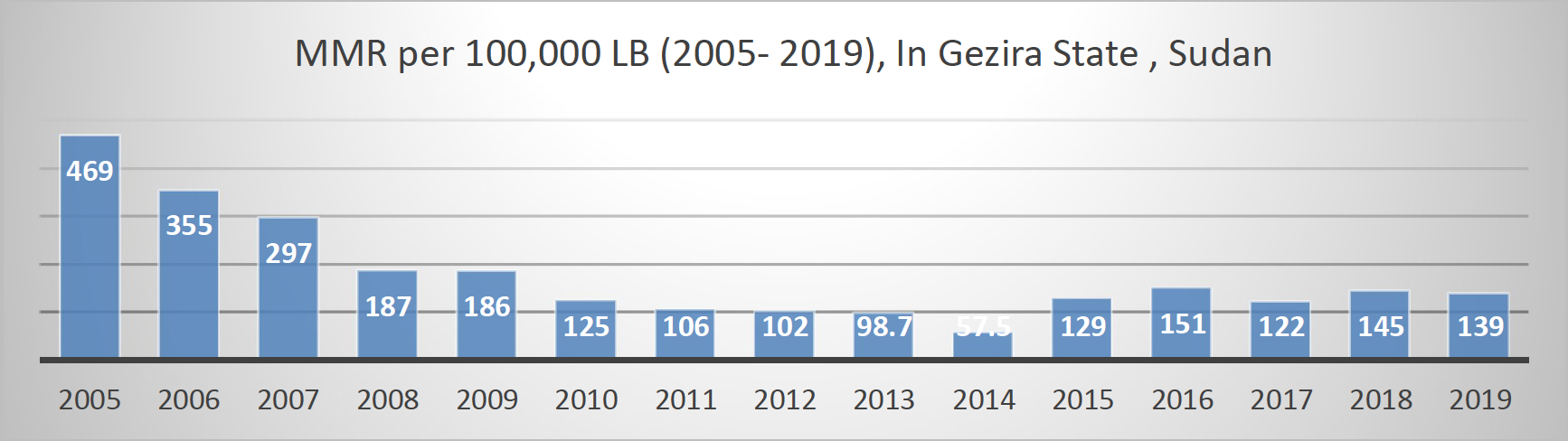
Figure 2: NMR per 1000 LB (2005- 2014), In Gezira State, Sudan
Discussion
The Safe Motherhood project is a classic example of how a socially accountable medical institution has positively responded to an identified societal need in a holistic manner and with measurable impact. Interventions lead to remarkable reduction in the maternal mortality ratio.
Experiences from successful maternal health programs showed that much of sufferings could be avoided if all women had the assistance delivered by a skillful health personnel during pregnancy and delivery, and access to emergency medical care when complications occurred (23). The Gezira community was appreciative and the performance of all individuals who contributed to make the event successful was recognized; their efforts were illustrated in colorful pictures.
For the future perspective, the successful programs may be replicable in developing countries with high maternal mortality, if adapted to specific cultural contexts. Many countries have achieved impressive declines in maternal mortality by implementing simple, cost-effective interventions within politically supportive environments. The initiative progress to Safe motherhood institute with sustainable programs.
For the sustainability of the project, recently the UGISMC progresses towards institution instead of Initiative project the Gezira Safe motherhood and Childhood Institute.
The project objectives are feasible, and the strategies are effective. This initiative has led to a remarkable reduction in the maternal mortality ratio and in the neonatal mortality ratio in Gezira State. The main problems which face the project are insufficient fund for mentainance of the initiative, rapid movement (turnover) of medical officers, difficulties of supervision of VMW and the high cost of equipment.
Conclusion
The Safe Motherhood project is a classic example of how a socially accountable medical institution has positively responded to an identified societal need in a holistic manner and with measurable impact. Interventions lead to remarkable reduction in the maternal mortality ratio. The safe motherhood project is a clear example of a number of projects that the medical school has initiated to improve the health status of the rural communities. This particular project, among other things, initiated the training of village mid-wives and facilitated their absorption into the government funded health system. The safe motherhood project is a classic example of how a socially accountable medical institution has positively responded to an identified societal need in a holistic manner and with measurable impact.
Authors
By Elhadi Ibrahim Miskeen1,2, MBBS, MD, Dr. Somia Khalafalla Abdulrahim2,3, MBBS, MD, Mohamed Elsanousi Mohamed2,3 JMPHE, MD, Ali Babikir Habour3, Yasir Mohamed Elhassan2,3 MD Ahmed Mustafa MD2 & Omer Ahmed Mirghani2,3 MRCOG
1. Department of obstetrics and Gynaecology, college of medicine, university of Bisha, Bisha 61922, P.O. Box 0011, Saudi Arabia
2. Department of obstetrics and Gynaecology, faculty of medicine, university of Gezira, Sudan.
3. Gezira institute for safe motherhood and childhood, University of Gezira, Sudan.


