EXECUTIVE SUMMARY
Despite progress made to reduce maternal mortality rates, roughly 300,000 women worldwide still die due to pregnancy-related complications every year, with significant variation by the country’s income level showing 180 deaths/100,000 live births in middle-income countries
(Seale, 2020). In Egypt, the Maternal Mortality Ratio (MMR) is estimated to be 37 per 100000 live births in 2017 (WHO, UNICEF, UNFPA, World Bank Group, and UN Population Division, 2019).
Maternal sepsis remains one of the major causes of maternal deaths worldwide, presenting 11 percent of the recorded deaths, and up to 15 women per 1000 births are affected in low- and middle-income countries (Alkema, Chou, Hogan, Zhang, Moller, Gemmill, Fat, et al., 2016). It is defined by the World Health Organization (WHO) as a life-threatening condition that arises when the body’s response to infection that causes injury to its organs during pregnancy, childbirth, after abortion, or during the post-delivery period (Leaper & Edmiston, 2017).
Our team believes that at the most basic, women deserve the fundamental right to live a healthy and safe life. And at the core of this is access to quality healthcare during pregnancy and childbirth. We believe that if we implement the right practice through the awareness of the health workers who need to be adequately trained, we can achieve change and witness a drop in MMR (Seale, 2020).
The ‘2016 WHO Global guidelines for the prevention of surgical site infection’ (SSI) were the leading effort against maternal sepsis, they developed evidence-based guidelines based on systematic reviews and present additional information in support of actions to improve practice, aiming to achieve standardization in practice addressing the issue (Leaper & Edmiston, 2017). However, recently in 2020, the WHO Global Maternal Sepsis Study (GLOSS) launched the STOP SEPSIS! awareness campaign. Studies show that its implementation was effective with regard to the recognition of respondents. There were significant changes in maternal sepsis identification and management (Brizuela, et al, 2020).
THE INNOVATION
Our team decided to integrate the 2016 recommendations into our facility standard practice, evidence-based practices have been highlighted as effective innovations. The emphasis has been on the rigor of the research methods used to produce evidence in support of innovation (Peterson, Haidar, Fixsen, Ramaswamy, Weiner, & Leatherman, 2018).
To select an innovation for use, there needs to be some steps: co-development of implementation capacity guided by the principles of Active Implementation. Our team was formed at the Ain Shams University Maternity Hospital (ASUMH) a tertiary hospital in Cairo, in collaboration with the ‘WHO Collaborating Center for Research Evidence for Sexual and Reproductive Health, the Department of Maternal and Child Health, and the Department of Health Policy and Management, Gillings School of Global Public Health, Department of Obstetrics and Gynecology, School of Medicine, and the Public Health Leadership Program, the University of North Carolina at Chapel Hill’, North Carolina USA.
ASUMH serves patients from all over Cairo & also referrals from other governorates in Egypt. We receive a heavy workload, with an average of about 16,000 deliveries per year. Four women health personals volunteered to join the Active Implementation team to study Implementation science from October 2018 till November 2019 and form the Implementation team.
From March 2019 till March 2020, our implementation project took place, the team worked on applying frameworks effectively and efficiently to affect change in practitioner behavior and organization’ system functioning to directly improve benefits to recipients. Our focus was directed towards our staff practice and behavior; our objective was to implement a new set of activities that we believe they can reduce the rate of maternal sepsis in our facility. We decided that educating our staff would be the best and most effective innovative solution (Horner, Sugai, & Fixsen, 2017).
We started by conducting a baseline observation to track our staff practice by recruiting independent observers from our volunteering medical students, who were given a detailed checklist on how to implement evidence-based practice in the labor and delivery setting (Leaper & Edmiston, 2017). Using the WHO 2016 recommendation model, we created a simple checklist to see how accurate our staff performance is. (Table 1) We also conducted a baseline online survey; asking the staff directly about their practice and their knowledge about the same set of recommendations (Leaper & Edmiston, 2017).
Looking into the results of the baseline observations, our team formed a couple of focus groups to start working on innovations that match the core components of an effective innovation; to be teachable, learnable, doable, and assessable in practice; and promote consistency across practitioners at the level of actual service delivery based on the need of the healthcare providers in our facility (Fixsen, Blasé, & Van Dyke, 2011).
Adopting the implementation mindset of continuous monitoring of multiple components as; staff selection, training, performance evaluation; facilitative administration; systems intervention. Our implementation team moved from the exploration phase into the staff training phase.1 We organized a couple of orientation meetings where we talked about our implementation goals, we clarified the gaps in our practice and what change we want to see happen. We designed a series of wall posters with the evidence-based recent recommendations that we placed in our facility to serve as a constant guide. (Figure 2)
OUTCOMES
Following the research implementation methods, our team used multiple-baseline designs (MBD) (Horner, Sugai, & Fixsen, 2017) to evaluate the efficacy of our intervention. The MBD, shown here, used to produce reliable information rapidly about the problems and solutions we subjected to research.
The data show changes in outcomes in each baseline before and after the introduction of an innovation. It allows simultaneous comparisons of post intervention scores with pre-intervention scores in the remaining baselines, thus controlling for general trends as practice effects and time-related events.
Figure 1 August 2019 March 2019
Figure 2 shows a collective summary of the posters the team designed to serve the innovation in our facility.
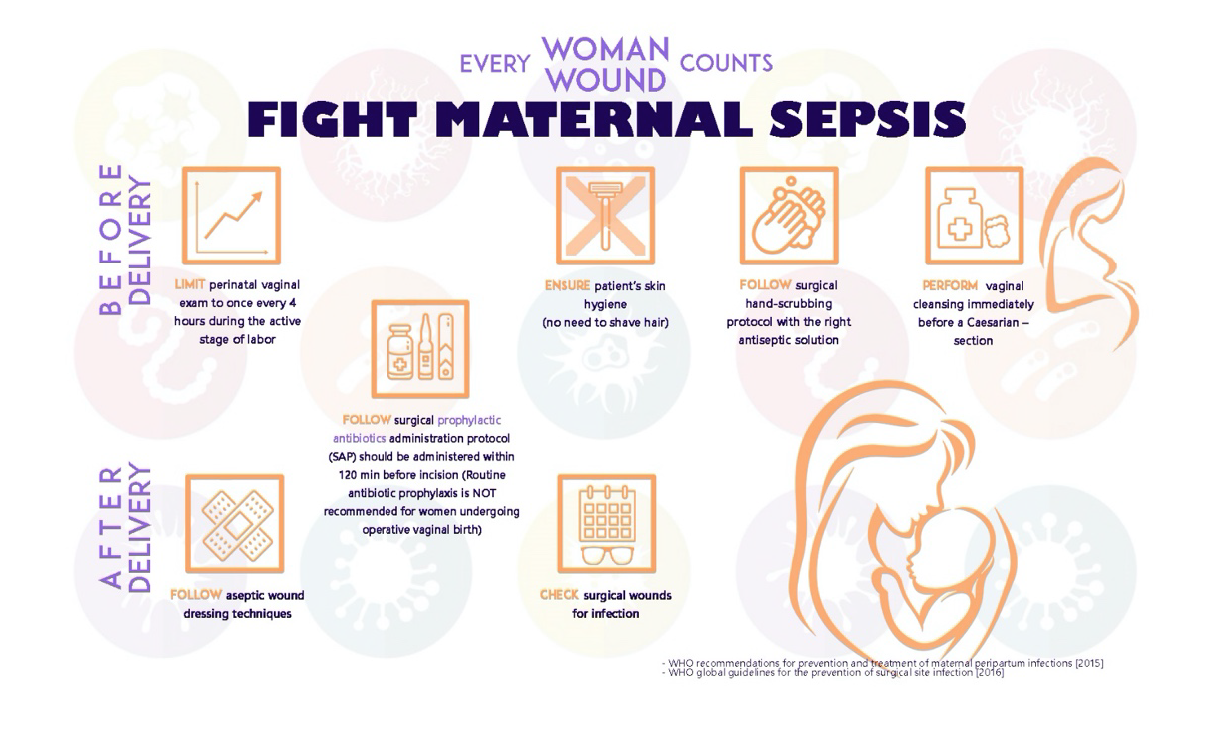
Table 1
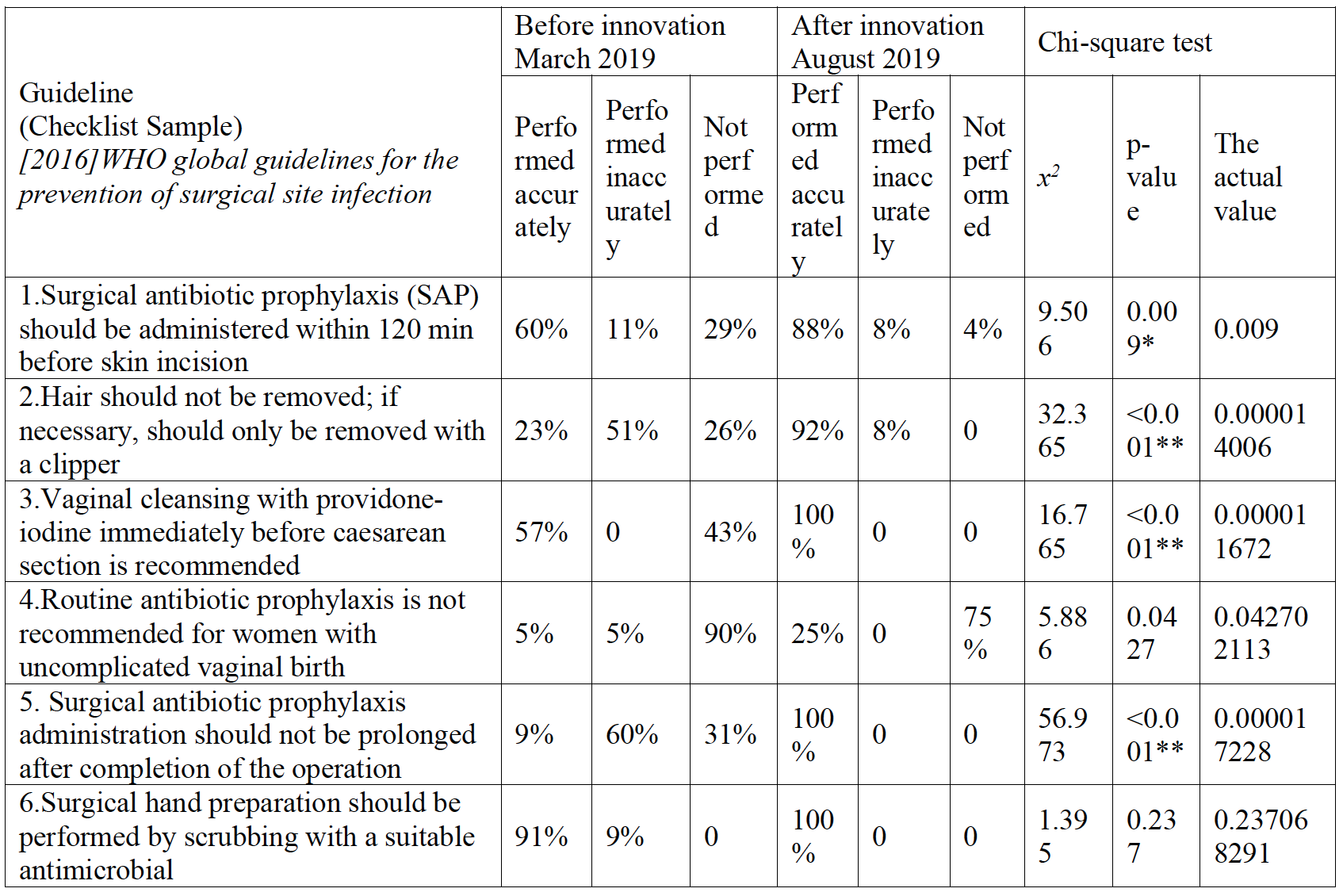
Total observations: 34
Using: Chi-square test;
p-value >0.05 NS; *p-value <0.05 S; **p-value <0.001 HS
Table 1 shows highly statistically significant improvement in after innovation observations compared to before innovation in compliance to WHO global guidelines for the prevention of surgical site infection 2016.
Comparing the data from our secondary observation; we see a significant change in staff performance. Referring to one guideline (Guideline 1 in Table 1); Surgical antibiotic prophylaxis (SAP) should be administered within 120 minutes before skin incision in operational Caesarian section delivery (Horner, Sugai, & Fixsen, 2017) - 60% of the total observed staff (34 personal) were accurately following the guideline before the innovation, while 88% followed it after the innovation. In contrast with Guideline 2 in Table 1, concerning the recommendation against hair removal before delivery (Horner, Sugai, & Fixsen, 2017), 23% of our staff were not aware of this guideline then 92% changed their practice after the innovation.
In attempting to use our innovation, the goal is to use its essential components with high fidelity thus change the organization as needed to fit the innovation. The status quo is powerful; fidelity is a lever for change (Horner, Sugai, & Fixsen, 2017).
Our implementation team support practitioners as they attempt to use innovations with fidelity first but we faced many challenges in that matter: we received minimal support from our organization leaders and other disciplines. Our improvement cycles were constantly interrupted by the resistance to change.
CONCLUSION
Our team planned to begin an improvement initiative, we are prepared to manage the change process and never lose sight of the original goal. When attempting to use an innovation in practice the expectation is that changes in related activities and routines will be required in ex-pected and unexpected ways. We believe that through learning and education, our staff can maintain the improvement cycles and constructively deliver the best-practice methods to our recipients. Our team is still working on keeping the improvement cycle; Plan, Do, Study, Act (PDSA) active in our organization. The PDSAC methods are helping us act in creative new ways to sustain our innovation. We look forward to new improvement strategies to contend with the acknowledged complexity inherent in our attempt to use innovation in practice.
Acknowledgments
This study was conducted by a group of volunteers; staff practitioners and medical students. We are very grateful to our mentors at UNC, Chapel Hill.
BIBLIOGRAPHY
Alkema, L., D. Chou, D. Hogan, S. Zhang, A. B. Moller, A. Gemmill, D. M. Fat, et al. Global, Regional, and National Levels and Trends in Maternal Mortality between 1990 and 2015, with Scenario-Based Projections to 2030: A Systematic Analysis by the Un Maternal Mortality Estimation Inter-Agency Group. [In eng]. Lancet 387, no. 10017 (Jan 30 2016): 462-74. https://doi.org/10.1016/s0140-6736(15)00838-7.
Brizuela, V. et al., Early evaluation of the 'STOP SEPSIS!' WHO Global Maternal Sepsis Awareness Campaign implemented for healthcare providers in 46 low, middle and high-income countries, BMJ Open 10, no. 5 (May 21 2020), https://doi.org/10.1136/bmjopen-2019-036338.
Fixsen, D. L., and Blasé, K. (2019). The Teaching-Family Model: The First 50 Years. [In eng]. Perspect Behav Sci, 42, no. 2 (Jun 2019): 189-211. https://doi.org/10.1007/s40614-018-0168-3.
Fixsen, D. L., Blase, K. and Van Dyke, M. (2011). Mobilizing Communities for Implementing Evidence-Based Youth Violence Prevention Programming: A Commentary. [In eng]. Am J Community Psychol 48, no. 1-2 (Sep 2011): 133-7. https://doi.org/10.1007/s10464-010-9410-1.
Horner, R. H., Sugai, G. and Fixsen, D. (2017). Implementing Effective Educational Practices at Scales of Social Importance. [In eng]. Clin Child Fam Psychol Rev 20, no. 1 (Mar 2017): 25-35. https://doi.org/10.1007/s10567-017-0224-7.
Leaper, D. J., and C. E. Edmiston. World Health Organization: Global Guidelines for the Prevention of Surgical Site Infection. [In eng]. J Hosp Infect 95, no. 2 (Feb 2017): 135-36. https://doi.org/10.1016/j.jhin.2016.12.016.
Peterson, H. B., Haidar, J., Fixsen, D,. Ramaswamy, B. Weiner, J., and Leatherman, S. (2018). Implementing Innovations in Global Women's, Children's, and Adolescents' Health: Realizing the Potential for Implementation Science. [In eng]. Obstet Gynecol 131, no. 3 (Mar 2018): 423-30. https://doi.org/10.1097/aog.0000000000002494.
Seale, Anna C. Frequency and Management of Maternal Infection in Health Facilities in 52 Countries (Gloss): A 1-Week Inception Cohort Study. [In eng]. Lancet Glob Health 8, no. 5 (May 2020): e661-e71. https://doi.org/10.1016/s2214-109x(20)30109-1.
WHO, UNICEF, UNFPA, World Bank Group, and the United Nations Population Division. Trends in Maternal Mortality: 2000 to 2017. Geneva, World Health Organization, 2019.


