Introduction
Today, factors such as the high level of expectations by the public, the increasing cost of health care, the recognition of social and environmental determinants of health, along with rampant inequity and poverty are further calls to action for society to become more socially accountable. Social Accountability and Interprofessional Education are being recognized by global health organizations such as the World Health Organization (WHO) as a practice and innovative strategy that will play an integral role in advancing universal health, equitable health care, and mitigating the global health workforce crisis. Nevertheless, in spite of a growing worldwide momentum in favor of the concept of Social and Interprofessional Education,1 and some outstanding achievements to implement them, there remains a large gap between good intentions and local government or institutional transformations.
Problem
Global organizations such as WHO, United Nations, and Global and Regional Associations have dedicated a tremendous amount of time and effort to successfully frame the global health conversations driven by health data, health priorities and trends, research, policy recommendations, global calls to action, and regularly convening global and regional health leaders, governments, and institutions to foster dialogue and learning.
In releasing global system and policy recommendations for local adoption and implementation, global organizations and associations recognize that adoption and implementation is complex and must take into account the local political and economic circumstances. In analyzing the limits of local change agents toward local innovation and collective action to adopt and implement global policy recommendations and calls to action, I am outlining the four factors that limit their implementation:
- Leaders at a local level must be prepared to better respond to local challenges and optimize local assets. Their relationships and experiences lead them to focus on local patterns they can observe and control directly. They need new skills and relationships with other stakeholders in the health sector to leverage complex change at scale.
- Resources for local change are constrained by a variety of factors, and each community experiences its own unique barriers. Local change agents require external technical guidance and sources of funding, not to replace, but to leverage local resources.
- Local action, while a powerful catalyst to people and day-to-day procedures and practice, is insufficient to support national and regional policies required for systemic transformation. Change agents at the local and regional levels need to understand the complex dynamics that work in regional, national, and global contexts and be able to interact with them to efficiently contribute to system change.
- Lessons learned in one local context are not accessible for system-wide analysis and continuous improvement for systemic change or application in other locales. The lack of system-wide evaluation also limits the evidence base for national and global policy change. Local Change Agendas need systems that collect data across a wide range of local contexts and systems-based analysis approaches to reveal patterns of systems change as it progresses.
Solution
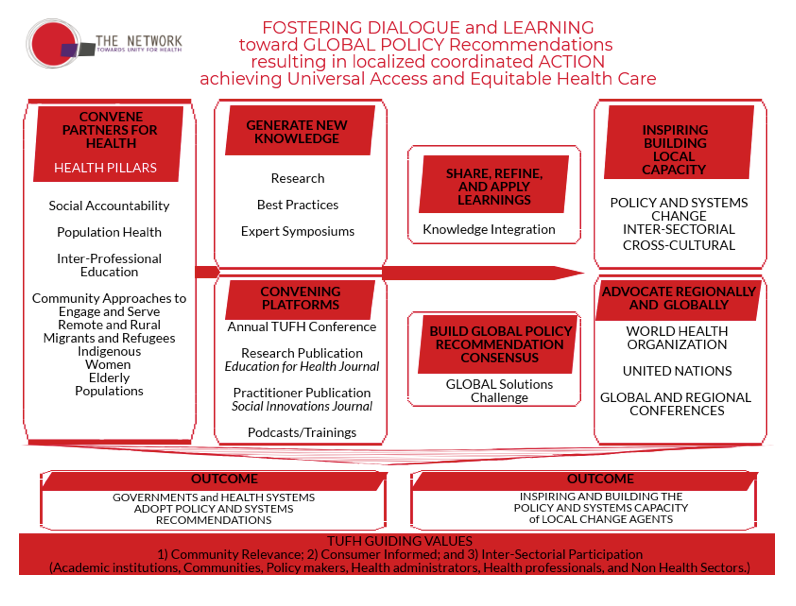
The beginning of moving global systems and policy change to local action starts with inspiring individuals and/or institutions through the sharing of ideas and success of others. Below outlines a three-step model, using network relationships as a strategy, to move global systems and policy recommendations toward local action.
Step 1: Knowledge Sharing
The Network: Towards Unity for Health (TUFH) is serving as a platform to share and distribute best practices and successes from countries around the world that have made progress in tackling and implementing ideas regarding Social Accountability and Population Health. The Network: Towards Unity for Health (TUFH), a non-state actor in official relations with WHO, believes that relationships are not only between organizations, but between people based around common interests. These relationships are not static, but rather grow and develop from the contributions of new members and future generations. A key element of The Network: TUFH is that it is not an insular organization. It is an ever evolving and inclusive network that embraces other organizations that are striving to create educational best practices, share community health approaches, and partner on research to develop the evidence for what works.
The articles on Social Accountability and Interprofessional Education contained in this edition represent case studies and success stories about how individuals and institutions are taking global policy recommendations and implementing and incorporating them into local policies and health system structures. Through the sharing of ideas and stories we inspire others to consider adoption and adaptation of the ideas and model for local change.
Step 2: Building Local Capacity
The road to global adoption and implementation is long and arduous. TUFH believes that the sharing of knowledge in the form of research and implementation best practices leads to inspiring local change agents to take action. Once inspired, local change agents can be supported by international and peer-to-peer policy and system change leaders and institutions whose primary role is to build their capacity and provide continual support and adaptation.
Building the capacity of local change agents takes the form of introducing a systems and policy change framework, providing formal opportunities to adapt the framework for a local context strategy, and providing continual support and adaption by, and with, other change agents across the globe. Networks, such as TUFH, being independent of local actors serve in the capacity of a convener and fill any knowledge gaps that might exist to create a culture that is supportive and learning based.
Step 3: Replication
The third step of moving global systems and policy change towards Universal Health and Equitable Health Care is to ensure there are community-to-community sharing platforms. As one community innovates and/or experiences success, networks such as TUFH, must ensure this knowledge is communicated and shared to other communities who have similar goals. Related to Social Accountability and Interprofessional Education, below outlines two possible courses for local replication via model adoption.
- Local actors work with local accreditation agencies to incorporate Social Accountability and Interprofessional Standards into their Accreditation Practices for medical, public health, and nursing schools.
- Local actors work with local medical, public health and nursing schools, and health systems to incorporate into their governance and advisory structures representatives from the Partnership Pentagram composed of Health Administrators; Policy Makers; Health Professionals; Academic Institutions; and Communities. These representatives will organically inform institution policies and strategies toward Social Accountability and Interprofessional Education Standards.
Conclusion
To bridge the gap between good intentions and government or institutional transformations, organizations such as TUFH must continue to serve as the link and connector between global policy organizations and local change agents such as policymakers, institutions, and associations who are doing the work on the ground. The work of TUFH and similar organizations continues to foster dialogue, build global consensus, grow the capacity of local change agents, and create platforms for knowledge to be shared and distributed. Collectively, we can change health care, but we first have to change the conversation.
1 Interprofessional education occurs when students, or members from two or more professions learn about, from and with each other to enable effective collaboration and improve health outcomes and services.


